Key Takeaways
- One in four dollars invested in healthcare are now spent on AI-related technologies.
- The EHR can act as a window into what parts of medical practice management systems can be automated.
- The future of medicine won’t rely squarely on AI, but will leverage the best aspects of automation and human input.
We’ve discussed the idea of creating systems to amplify your unique value to the patient. We’ve explored removing activities that can be managed by delegated staff or specific systems. And we’ve reviewed meeting selected KPIs by starting with the “why.”
Underpinning all of these concepts is having the right technology in place. It’s an aspect of medical practice management systems that’s easy to take for granted. For all of the data input complaints doctors throw at EHRs, can you imagine a day in a busy practice without one?
One contemporary innovation taking our industry by storm is AI. One in four dollars invested in healthcare is now spent on AI-related solutions. If this keeps up, the World Economic Forum (WEF) projects the healthcare AI sector will be worth almost $188 billion by 2030.
As AI use snowballs within healthcare, how can your practice anticipate getting the most out of intelligent technology?
With AI presenting existential challenges and opportunities to medical practice management, I propose people—not algorithms—will be needed more than ever to guide care in the right direction.
The Enduring Role of Healthcare Professionals in the Age of AI
In the past, physicians had unique knowledge, access to information, and thought processes related to care delivery. Doctors were quite literally the only ones who read—or often had access to—the textbook.
With the advent of the internet, everything changed. Information became a readily accessible commodity. Virtually anyone with broadband access could hop on the World Wide Web and find relevant facts, figures, and step-by-step instructions that could inform their health journeys.
But facts aren’t insights. They’re static, raw knowledge materials that must be harnessed in the right way to make an impact. Additionally, not all data points floating in the ether are valid. The online world is full of inaccurate findings, outdated instructions, and misleading sources.
That’s where the physician will always play a unique role—in looking patients in the eye, synthesizing real-world experience with best practices, and delivering high-quality care that only a trained professional can. And it doesn’t stop with doctors. Front-of-office staff lend incredible value to the function of a medical practice by assisting individuals with a personal touch—helping people navigate their care and feel heard throughout their health journeys.
Determining Tasks for AI-Powered Medical Practice Management Software
Defining the activities involved in a typical encounter and comparing humans to what AI will likely provide helps us to understand where humans will deliver enduring value. Let’s dive into this concept with one of the cornerstones of medical practice management systems: the EHR.
Some EHR-related tasks that AI will help automate inevitably include:
- Aggregate chart information from prior encounters, outside consults, labs, imaging, testing, and third-party data as a pretext to the encounter
- Generate chart findings during the medical encounter based upon natural language communications
- Transcribe the assessment and associate diagnosis codes
- Enter and transmit the orders associated with the encounter.
What won’t AI feasibly take off of human hands? The very substance of patient-provider relationships. It can’t create context and meaning based upon the patient’s history and medical data. It can’t provide nuanced judgment regarding treatment alternatives and the necessity of further intervention. And, perhaps most importantly, it can’t listen to and empathize with human beings.
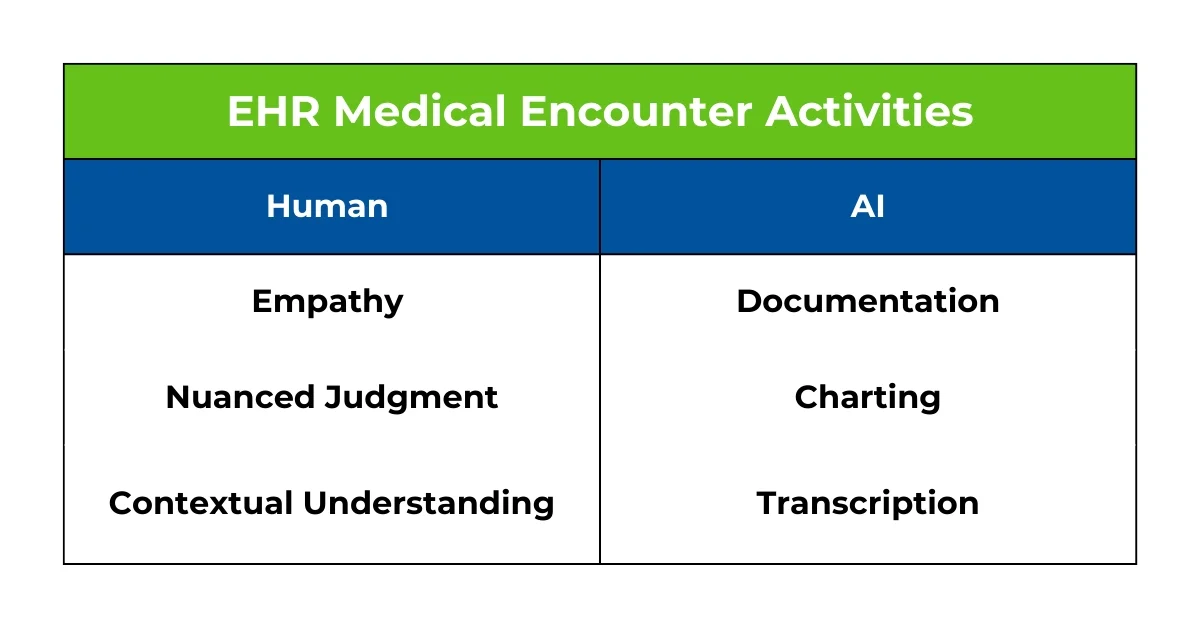
Put simply, much of the administrative side of caring for patients will no longer be required of the physician or even staff in the near future. Yet there are many human activities— including creating narrative understanding for the patient, providing nuanced judgment, exercising medical and surgical skills, and, most importantly, listening and empathizing with the patient—where AI will never usurp our role.
Learn more about successful EHR implementation with our comprehensive guide
Combining Human Ingenuity With AI to Advance Care
Though we’ve covered the subject of AI use within the private practice environment in a siloed fashion—pitting tasks AI could take on vs. those that are human-exclusive—the reality is that intelligent technology is going to be used most effectively by and for humanity.
An easily understandable analogy to how I imagine the AI-provider relationship evolving is the experience with “Centaur” (or “Cyborg”) chess teams—a hybrid form of chess which includes humans using computer chess engines. Human strategic thinking and creativity paired with the computational power and accuracy of chess engines can sometimes yield better results than either humans or computers alone.
However, as neural network-based engines have evolved, the advantage once experienced by Centaur teams has narrowed or in some instances surpassed by the newer computer chess engines.
That’s where healthcare deviates from this analogy. Consistent human interactions required when caring for patients will likely never be replaced. Part of preparing for the future is embracing where AI or automated systems can help, creating the space to amplify the uniquely human activities.
A New Set of Fusion Skills
Just as AI is conforming naturally to its intuitive role as an ally, not replacement, in the healthcare context, providers themselves will need to adapt to a new normal to get the most out of intelligent technology. This will involve cementing a few key skills, including:
- AI fluency: The ability to work alongside AI systems, understanding their strengths and limitations, and knowing when to rely on AI and when to apply human judgment.
- Data literacy: The skill to interpret, analyze, and make decisions based on data insights generated by AI tools. This includes understanding data trends, anomalies, and patterns identified by AI algorithms.
- Critical thinking and ethical decision-making: Assessing ethical implications of AI decisions and accounting for implicit bias, ensuring that medical practice management systems are used responsibly and in a way that aligns with human values.
- Adaptive learning: Learning continually and adapting to new AI tools and technologies—staying updated with the latest developments in AI and incorporating them into daily tasks.
- Creative problem-solving: Using AI to explore new ideas, generate creative solutions, and innovate in ways that weren’t possible previously. This involves leveraging AI for tasks like design, marketing, and product development.
- Technical proficiency: While not all fusion skills require deep technical knowledge, having a basic understanding of AI technologies—such as machine learning, natural language processing, and robotics—can enhance one’s ability to collaborate with AI systems effectively.
- Communication and interpretation: Explaining and interpreting AI outputs to non-experts, making complex AI-driven insights understandable and actionable for broader audiences.
Imagining Medical Practice Management Software of the Future
Fusion skills are increasingly important as AI becomes more integrated into various aspects of work and life—enabling individuals to maximize the benefits of AI while maintaining human control and oversight.
Thus, actively enabling automation and AI services to relieve us of mundane activities is an easy first step. Medical practice management companies like WRS Health have been on the vanguard of streamlining routine tasks for some time now, and will continue to be instrumental in simplifying private practice operations in years to come.
Find Out More About Our Advanced EHR

Dr. Lawrence Gordon, MD
He is a practicing Otolaryngologist and the founder of ENT Specialty Care located in Goshen, NY. He is also the CEO and Founder of WRS Health. The software is an all-in-one platform, designed by physicians, providing clinician-centered workflow solutions to continually improve and grow your practice.





 QUICK CHARTING
QUICK CHARTING NOTE
NOTE MEDICATION
MEDICATION PATIENT
PATIENT BILLING
BILLING RISK
RISK MARKETING
MARKETING MIPS
MIPS