Key Takeaways
- AI in healthcare helps practices submit cleaner claims and get paid faster.
- Payers are already using AI for claims, and providers must adapt to stay competitive.
- Integrating AI into EHR workflows improves accuracy, efficiency, and compliance.
- Leverage WRS Health’s AI-enabled EHR to stay ahead in medical billing.
Artificial intelligence is no longer a “future” topic in healthcare—it’s here now. From ambient scribes to coding guidance, AI is changing how medical practices operate day to day. These features also affect how practices align with partners and payers.
Payers already invest heavily in AI-driven analytics to accelerate claims decisions, automate prior authorizations, and predict patient risk. These tools help insurers process massive volumes of information quickly, spot patterns, and act with a level of efficiency manual workflows can’t match.
Practices that avoid AI fall behind. While insurers speed approvals and cut costs, many provider offices still chase claim rejections, redo documentation, and struggle to keep up. The gap between payers and providers grows wider every year.
Practices asking “how will AI help change EHRs?” and updating their systems now are better positioned for success. By weaving AI into everyday operations, they can improve how they manage claims, streamline workflows, and align documentation with payer expectations from the start.
Table of Contents
- Key Takeaways
- Smarter EHRs With AI: From Recordkeeping to Revenue Protection
- AI-Driven EHRs That Anticipate Needs and Align With Payers
- What Payers Are Already Doing—and Why It Matters
- The Practice Perspective: Where AI Makes the Biggest Impact
- Overcoming Implementation Hurdles
- The Long-Term Path: Aligning With Value-Based Care
- The AI Divide: Practices Can’t Afford to Stay on the Sidelines
- Related Posts
Smarter EHRs With AI: From Recordkeeping to Revenue Protection
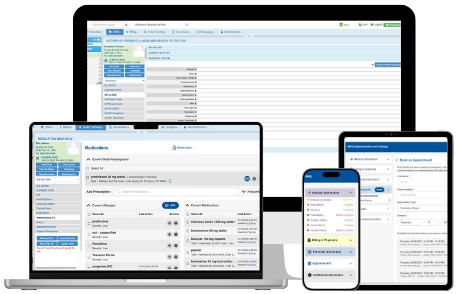
An electronic health record is the operational hub where clinical care, billing, and communication meet. So, how is AI used in EHR systems to make them more effective? The answer is automation and intelligence that extend beyond standard reports.
AI provides real-time coding support, analyzing documentation patterns and payer history to suggest the most accurate codes. It scans for missing or inconsistent details before submission so practices correct errors before rejections occur. Over time, it adapts by learning from payer responses, improving documentation and coding so each claim is cleaner than the last.
Instead of serving only as storage, the EHR becomes an active part of the revenue cycle. By preventing errors upfront, AI reduces administrative work, speeds reimbursement, and stabilizes financial health—an essential advantage when insurers themselves are already powered by AI.
AI-Driven EHRs That Anticipate Needs and Align With Payers
Practices are using AI to improve electronic health records, and in doing so, support their growth and sustainability goals. AI makes EHR systems more intuitive. Instead of clicking through multiple screens to find the right code or form, the system anticipates what you need during the patient encounter.
If a specific insurer requires additional detail for a procedure, the EHR prompts for it before the visit note is complete. These predictive capabilities keep documentation aligned with payer expectations, minimize back-and-forth, and make workflows cleaner and faster. Over time, claims are not just submitted more quickly—they’re submitted correctly the first time.
What Payers Are Already Doing—and Why It Matters
Insurers already hold the technological upper hand. As Healthcare Dive reports, payers are using AI in claims review to accelerate decisions—while providers struggle to catch up. AI agents process straightforward claims instantly and escalate only complex ones to human reviewers. This gives payers a speed and accuracy advantage.
Practices without AI risk falling further behind. Providers still enter codes, check eligibility, and correct denials manually, while insurers leverage automation to eliminate those steps. Without similar tools, practices operate at a constant disadvantage in both speed and accuracy.
The Practice Perspective: Where AI Makes the Biggest Impact
Adopting AI in healthcare means practices are positioned to match insurers’ technology and protect their revenue cycles. Imagine a system that automatically checks a claim against every payer’s rules before submission. Instead of finding out two weeks later that information was missing, you know instantly and can fix it on the spot.
AI can also alert staff to claims sitting too long without payment, prompt for quality measure documentation during a visit, and predict which procedures are most likely to face payer scrutiny. In each case, the goal is the same: reduce friction, speed reimbursement, and make processes more predictable.
Overcoming Implementation Hurdles
Change can be uncomfortable, especially when it affects many people and processes. Practices might assume adopting AI means starting over completely, or enduring rigorous training that disrupts operations. In reality, taking the time to plan and implement AI-powered features now can save time, and money, in the future.
The key to a seamless rollout is selecting a vendor who offers customized solutions and takes time to understand your practice. Start with the areas that will have the greatest impact. For many, this means focusing on claim scrubbing, coding assistance, and documentation prompts.
Training should be phased in, allowing staff to master one capability before introducing another. It’s also essential to monitor performance—track denial rates, turnaround times, and user adoption to ensure the investment is delivering measurable results. A partner that offers integrated AI features like WRS Health is critical to avoiding piecemeal solutions that disrupt workflows.
The Long-Term Path: Aligning With Value-Based Care
AI’s potential isn’t limited to claims management. As more payers move toward value-based reimbursement, AI can help practices identify at-risk patients, close care gaps, and track outcomes against quality measures. This positions providers to succeed in reimbursement models that reward results rather than volume.
Insurers are already combining claims, clinical data, and social determinants of health to manage populations. Practices that use AI to do the same can have more informed conversations with payers, negotiate from a stronger position, and ensure they’re meeting the metrics that drive payment in value-based arrangements.
The AI Divide: Practices Can’t Afford to Stay on the Sidelines
AI is no longer an emerging technology. Payers are using it now to improve accuracy, reduce costs, and speed up decisions, rendering it a business necessity. Practices that adopt AI for EHR and claims management can:
- Submit cleaner claims that meet payer requirements from the start.
- Reduce denials and shorten reimbursement timelines.
- Improve staff efficiency by automating repetitive tasks.
- Strengthen their position in value-based care arrangements.
The question isn’t whether AI will affect your practice—it’s whether you’ll use it to your advantage.





 QUICK CHARTING
QUICK CHARTING NOTE
NOTE MEDICATION
MEDICATION PATIENT
PATIENT BILLING
BILLING RISK
RISK MARKETING
MARKETING MIPS
MIPS