Key Takeaways
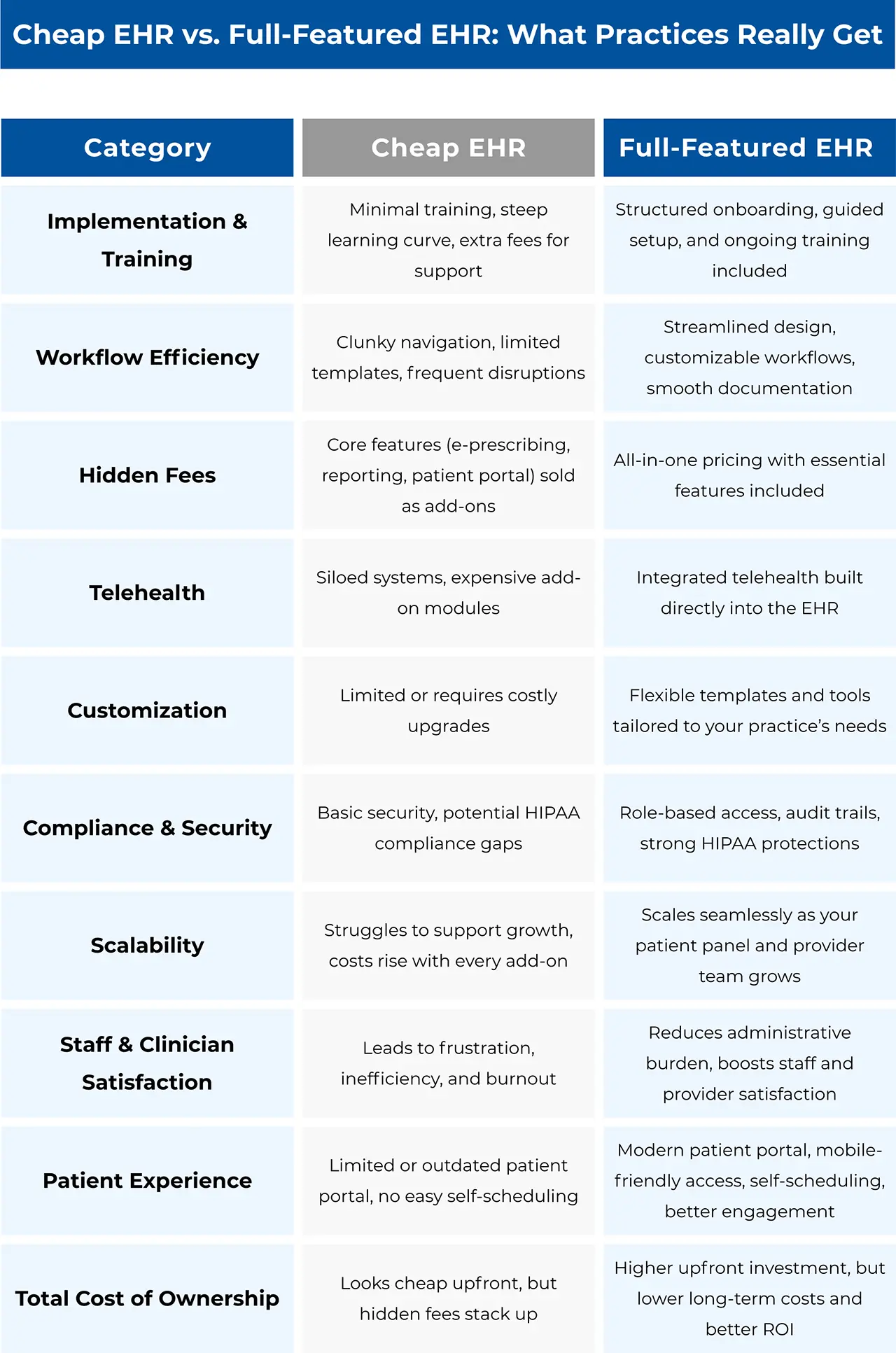
- When evaluating an EHR system, it’s critical to look beyond the sticker price.
- The real cost of a cheap EHR shows up in inefficiency, staff burnout, compliance risks, and patient dissatisfaction.
- A robust, scalable EHR might require a higher initial investment, but it pays off by streamlining workflows, improving patient care, and avoiding a cycle of add-ons and hidden fees.
- Discover 5 secrets to an easy EHR transition.
At first glance, a cheap EHR might seem like the perfect solution for a growing practice. After all, why spend more when you can start with something “affordable”? But many practices soon discover that what looks budget-friendly on paper often leads to frustration, hidden fees, and expensive workflow disruptions.
If you’re weighing options like an affordable EHR for small practices or even asking, “is there a free EHR?”, it’s important to understand the full picture of what you’re actually paying for.
Let’s break down the real costs of starting with a system that only appears to save you money.
Table of Contents
- Key Takeaways
- The Real Price of Implementation
- Workflow Disruption: The Cost You Don’t See on the Invoice
- The Nickel-and-Dime Trap: Add-Ons and Hidden Fees
- Telehealth and Siloed Charges
- How Much Does an EHR Cost, Really?
- What a Full-Feature EHR Provides From Day One
- Choosing Wisely: Invest in Long-Term Value
- Related Posts
The Real Price of Implementation
Implementation is often where the first surprise costs show up. With a cheap EHR, onboarding is typically minimal, with little guidance beyond the basics. That means:
- Limited training that leaves staff guessing how to use the system efficiently
- Extra hours spent troubleshooting instead of caring for patients
- Additional charges for “premium” training sessions or extended support
The result? Extended adoption timelines and frustrated staff who struggle to fully embrace the system. According to KLAS Research, with poor training, only 36% of end-users said they were satisfied with the EHR. Without buy-in, successful implementation becomes nearly impossible, and what once seemed affordable quickly turns into a drain on both efficiency and morale.
Experienced EHR and AI technology vendors like WRS Health address these challenges with free implementation and comprehensive, full-staff training.
Workflow Disruption: The Cost You Don’t See on the Invoice
A clunky or limited EHR both slows down your day and changes the way your entire team works, often for the worse.
- Documentation bottlenecks: Cheap systems may not offer practice-specific templates or tools, forcing providers into time-consuming manual work.
- Inefficient billing workflows: Gaps in revenue cycle management lead to delays and denials.
- Staff burnout: Extra clicks, repetitive data entry, and broken workflows eat up clinical time and increase turnover.
Every minute wasted navigating poor design is a minute not spent with patients. Those “lost minutes” translate directly into lost revenue and declining quality of care.
The Nickel-and-Dime Trap: Add-Ons and Hidden Fees
Many practices start with a low sticker price, only to realize that core features are locked behind extra fees. Common examples include:
- Advanced reporting or analytics
- Customization of templates and forms
- Secure messaging or patient portal access
- E-prescribing, especially for controlled substances
What looked like an “affordable EHR for small practices” can quickly balloon into a system that costs more than premium solutions without delivering the same value. WRS Health’s full-featured EHR system solves these pain points by delivering reporting, e-prescribing, and customization capabilities along with patient portal access and more, right from the start.
Telehealth and Siloed Charges
Today, telehealth is non-negotiable for patient access. But with a cheap EHR, you may find telehealth tools are sold as costly add-ons, or worse, not available at all.
This could force your practice into fragmented workflows, juggling separate systems for scheduling, documentation, billing, and telehealth. Not only does this add unnecessary subscription costs, but it also increases compliance risks and reduces efficiency.
How Much Does an EHR Cost, Really?
So, how much does an EHR cost? The answer depends not just on the sticker price, but on the total cost of ownership (TCO):
- Direct costs: Licensing, setup, support, and training
- Indirect costs: Staff productivity losses, patient no-shows, billing errors, and turnover from burnout
- Growth costs: Paying extra for every new provider, feature, or integration you need as your practice expands
What a Full-Feature EHR Provides From Day One
Unlike limited systems that leave you to figure things out, a robust EHR invests in your success right from the start. This means:
- Free implementation support – EHR implementation success can have lasting impact on a medical practices’ satisfaction. An integrated EHR setup ensures your workflows, templates, and settings are configured correctly from day one. It is helpful to know what a successful implementation looks like as it is one of the signs of having the right EHR vendor.
- Comprehensive training – With proper training, a whopping 83% of end-users report satisfaction compared to only 36% without it. You know you are getting a value-for-money EHR when your team gets hands-on training sessions (not just a quick demo).
- Data migration included – Patient records, demographics, and historical notes are moved over smoothly without extra costs or disruption.
- Practice-specific customization – Templates, order sets, and documentation tools are tailored to your specialty and workflow, reducing clicks and boosting efficiency.
- Ongoing support at no extra charge – Access to responsive customer support and continuous training keeps your staff up to speed as your practice grows. The right EHR partner doesn’t disappear after the contract is signed, they’re there every step of the way to ensure lasting success.
The difference is clear: instead of being nickel-and-dimed for the basics, you get a partner committed to your long-term success.
Choosing Wisely: Invest in Long-Term Value
Instead of asking “is there a free EHR?”, ask:
- Will this system scale as my practice grows?
- Does it come with practice-specific tools?
- Are telehealth, patient engagement, and reporting built in or sold separately?
- How much support and training are included?
An inexpensive EHR may look attractive today, but the hidden costs such as implementation struggles, workflow disruptions, add-ons, and siloed telehealth charges can quietly drain your practice’s resources.
Investing in a robust EHR built specifically for your practice is more about value than cost. The right solution fuels your practice’s growth, improves clinician satisfaction, and ensures patients get the care they deserve.





 QUICK CHARTING
QUICK CHARTING NOTE
NOTE MEDICATION
MEDICATION PATIENT
PATIENT BILLING
BILLING RISK
RISK MARKETING
MARKETING MIPS
MIPS